Ovulation timing is one of the biggest factors that shape your menstrual cycle and your chances of getting pregnant. A common question many women ask while trying to conceive is: “If I ovulate late, can I still get pregnant?”
The answer is yes. Late ovulation pregnancy success is absolutely possible. Ovulation can shift your cycle length, which might delay your period, but conception can still occur as long as ovulation happens and sperm meets the egg at the right time.
Many women panic when their period doesn’t arrive on time or when ovulation tests seem inconsistent, but late ovulation doesn’t necessarily mean a fertility issue. Understanding why it happens, how to track it, and when to seek help can make your trying to conceive (TTC) journey much more reassuring.
Understanding Ovulation and Why Timing Matters
Your menstrual cycle is divided into four key phases: the menstrual phase, the follicular phase, ovulation, and the luteal phase. Ovulation is the moment your ovary releases a mature egg, and it’s the most fertile point of your cycle.
After ovulation, the luteal phase begins. This phase typically lasts 12-14 days and ends when your period starts.
Here’s the key: Your luteal phase length stays consistent, but your follicular phase (before ovulation) can vary. When ovulation happens later, your entire cycle gets longer—but that can be normal.
That’s why late ovulation means a late period, it’s not that your luteal phase changed, but that ovulation occurred later than usual.
What Causes Late Ovulation?
There are several reasons ovulation may occur later than expected in a given cycle. Some are temporary and harmless, while others may reflect hormonal shifts that need attention.
Lifestyle Factors
Your body is sensitive to lifestyle changes. Stress, illness, lack of sleep, travel, or even intense workouts can delay ovulation. The brain and ovaries communicate through hormonal signals, and stress hormones like cortisol can interfere with that process, causing a delay.
If you’ve had a stressful month or changed your daily routine, a late ovulation cycle might be your body’s way of adapting before returning to normal the next month.
Health Conditions
Certain health issues can influence your ovulation timing. Polycystic ovary syndrome (PCOS), thyroid disorders, perimenopause, or recently coming off hormonal birth control can all delay ovulation.
Late Ovulation and PCOS
Polycystic ovary syndrome (PCOS) is the most common cause of consistently late or irregular ovulation. Women with PCOS often:
- Ovulate unpredictably (CD20–40+)
- Have multiple LH surges without ovulation
- Need more sensitive tracking to catch subtle LH rises
If you have PCOS: Quantitative OPK tracking with Premom is especially valuable, as it can detect hard-to-read LH levels that traditional ovulation test strips miss.
For example, when you stop birth control pills, it may take a few months for your body to reestablish its natural hormonal rhythm. Similarly, thyroid or PCOS-related hormone imbalances can cause irregular ovulation patterns that vary from cycle to cycle.
Natural Cycle Variation
Even in healthy women, cycles aren’t always a perfect 28 days. Having a 31- or 35-day cycle occasionally is normal and often just reflects a longer follicular phase. A single late ovulation cycle doesn’t mean something is wrong, it’s simply your body’s natural variation.
Does Late Ovulation Always Mean a Late Period?
Yes, ovulation determines when your period arrives. Once you ovulate, the luteal phase clock starts ticking, and your period will typically come 12–14 days later.
For example, if ovulation happens on cycle day (CD) 21 instead of CD14, your period might come around CD35. That’s why late ovulation means a late period, not necessarily a missed one.
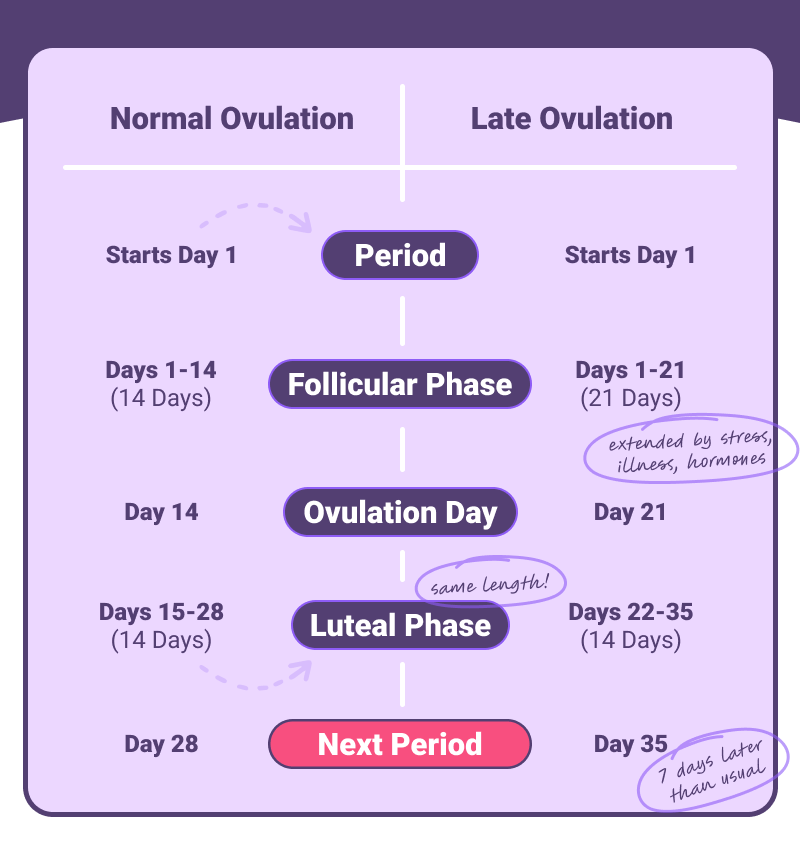
Here’s what this looks like in practice:
Cycle Example 1: Normal Ovulation
- Period starts: Day 1
- Follicular phase: Days 1-14 (14 days)
- Ovulation: Day 14
- Luteal phase: Days 15-28 (14 days)
- Next period arrives: Day 28
Cycle Example 2: Late Ovulation
- Period starts: Day 1
- Follicular phase: Days 1-21 (21 days) ← Extended by stress/illness/hormones
- Ovulation: Day 21
- Luteal phase: Days 22-35 (14 days) ←Same length!
- Next period arrives: Day 35 ← 7 days later than usual
The key: Your luteal phase stays consistent (12-14 days). When ovulation is delayed, your period is automatically delayed by the same amount.
If your cycles occasionally run long but remain consistent in pattern, there’s usually no cause for concern. However, if you notice frequent changes or cycles longer than 35 days, it’s worth tracking more closely and consulting a provider if it persists.
(Tip: The Premom app automatically adjusts your predicted period date once ovulation is detected, so you can avoid that “late period panic.”)
How Late Ovulation Affects Pregnancy Chances
Fertility chances with late ovulation
The great news is that pregnancy after late ovulation is absolutely possible. If ovulation occurs and you have well-timed intercourse during your fertile window, conception can happen, no matter which day it falls on.
However, identifying that fertile window is key. The fertile window typically includes the five days before ovulation and the day of ovulation itself. So if ovulation happens on day 21 instead of day 14, your fertile window simply shifts later.
That’s why it’s essential to track ovulation signs rather than relying on calendar predictions. Ovulation tests and PdG kits can help ensure you’re not missing that later window to have sex.
Egg quality and luteal phase length
Some studies suggest that late ovulation, especially when cycles are longer than 35 days, may occasionally be linked with slightly reduced egg quality. This can make implantation less likely, but it’s not a guaranteed issue.
What matters more is whether your luteal phase remains long enough (ideally 12–14 days) to support implantation. If the luteal phase is shortened to fewer than 10 days, implantation may not occur successfully, which is one reason tracking PdG and BBT after ovulation is so valuable.
When to have sex if ovulation is late
If ovulation is delayed, your fertile window simply shifts later, too. Continue having intercourse every other day once you start seeing rising LH levels or changes in cervical mucus.
The key takeaway: late ovulation doesn’t harm your fertility if you’re timing intercourse correctly. What matters most is when ovulation happens, not how long your cycle is.
Stop guessing when ovulation happens. Track your unique cycle with Premom’s AI-powered charts—designed for irregular patterns and late surges. Start tracking for free on the Premom app.
How to Track Ovulation If It’s Late or Irregular
Tracking ovulation accurately is especially important when cycles vary from month to month. Here are some effective strategies to help pinpoint late ovulation and improve your chances of conception.
Test More Frequently
If your periods are unpredictable, consider testing for LH twice per day during your expected fertile window. Some surges happen quickly and can be missed with once-daily testing.
Combine Tracking Methods
Combining LH, BBT, PdG, and cervical mucus (CM) tracking gives you a complete fertility picture. CM offers daily clues about approaching fertility, along with LH tests. While BBT and PdG strips can help verify if ovulation has likely happened.
Traditional OPKs show a simple “positive” or “negative” line. But quantitative OPKs (like those used with Premom) measure your exact LH level in mIU/mL—giving you numeric data instead of guesswork. This is especially helpful for detecting subtle surges in women with PCOS or naturally low LH. This helps catch subtle surges that traditional strips may overlook, especially in women with PCOS or low baseline LH
When to Be Concerned About Late Ovulation
A late ovulation cycle here and there is perfectly normal, but if it happens repeatedly or comes with other symptoms, it may signal an underlying issue worth investigating with your provider.
Periods Consistently Longer Than 35 Days
If your cycles are regularly extending beyond 35 days, it could mean that ovulation isn’t happening consistently. This can be caused by PCOS, thyroid dysfunction, or other hormonal imbalances that delay follicle development.
Luteal Phase Shorter Than 10 Days
A short luteal phase can make implantation difficult and increase the risk of early pregnancy loss. If you notice your luteal phase is consistently under 10 days, bring it up to your healthcare provider. They may recommend progesterone testing or treatment options.
No LH Surge Across Multiple Cycles
If you’ve tracked for several months without detecting an LH surge, it’s worth getting evaluated. This could indicate anovulation (no ovulation), which is common with PCOS or perimenopause. Blood tests and ultrasounds can help confirm what’s happening hormonally.
Heavy Bleeding or Irregular Patterns
Heavier periods, mid-cycle spotting, or irregular bleeding patterns may suggest endometrial or hormonal changes that need a closer look. A doctor can help identify the cause and discuss treatment options to support your fertility.
Late Ovulation vs. Anovulation
Late Ovulation vs. Anovulation: What’s the Difference?
Late ovulation means ovulation occurs later than typical (after CD21) but still happens. Signs include:
- Delayed positive OPK
- BBT rise later in cycle
- Confirmed ovulation via PdG test
Anovulation means no ovulation occurs at all. Signs include:
- No positive OPK throughout the cycle
- No BBT temperature shift
- Negative PdG tests
- Very long or very short cycles
Why it matters:
Late ovulation still offers a chance for pregnancy each cycle. Anovulation does not—and requires medical intervention.
If you’re unsure which you’re experiencing, consistent tracking with Premom can help identify patterns to discuss with your healthcare provider.
Natural Ways to Support More Regular Ovulation
While not every case of late ovulation needs medical intervention, certain lifestyle and nutrition changes can help support hormone balance and promote more predictable cycles.
- Focus on Balanced Nutrition
Eat nutrient-rich foods that support reproductive health, such as leafy greens, salmon, avocados, and whole grains. Nutrients like folate, vitamin D, and omega-3 fatty acids are known to support hormone regulation and egg health. - Try Supplements That Support Cycle Health
Supplements like inositol can help promote more regular ovulation, especially in women with PCOS or irregular cycles. Omega–3 DHA supports hormonal balance, and a prenatal vitamin ensures your body has baseline nutrients for conception. - Manage Stress and Lifestyle Habits
High stress, poor sleep, or overexercising can disrupt your cycle. Relaxation practices like yoga, mindfulness, or even journaling can make a big difference. - Prioritize Sleep and Recovery
Getting 7–9 hours of quality sleep each night helps maintain healthy cortisol and reproductive hormone levels. Your body’s natural repair and regulation happen during sleep. - Track Your Cycle Consistently
Tracking helps you identify trends and catch shifts earlier. The Premom app brings together OPKs, PdG tests, and BBT charts so you can see the full cycle picture, especially helpful for spotting late or subtle ovulation surges.
How Premom Helps Detect Late Surges
One of the most frustrating parts of late ovulation is not knowing when your fertile window is actually open. This is where Premom can make tracking easier and more accurate.
The app uses advanced algorithmic insights to analyze your hormone data, so even if your LH surge is short or delayed, the app’s AI–based charting helps catch it. It’s especially useful for women with unpredictable cycles, where timing can change month to month.
Using the Easy@Home LH & PdG Combo Kit gives you a reliable, science-backed way to monitor both the ovulation trigger (LH) and luteal phase rise of progesterone (PdG). When used together in the Premom app, these tools provide full-cycle insight, from your LH rise before ovulation to your PdG tracking afterward.
The combination of visual graphs, automatic ratio detection, and post-ovulation verification removes the guesswork and helps you plan intercourse with confidence.
Many women who experienced late or hard-to-detect surges share success stories in the Premom community, finding reassurance and real results after switching to smarter, data-driven tracking.
Final Thoughts
Experiencing late ovulation can feel confusing and sometimes discouraging, especially when you’re eagerly waiting for that positive LH test or your period. But remember, late ovulation pregnancy success is completely possible.
The key is knowing your body’s rhythm, testing consistently, and using the right tools to track ovulation accurately. Whether your ovulation happens on day 14 or day 24, Premom adapts to your unique pattern. Start tracking today and take the guesswork out of getting pregnant.
Whether your ovulation happens on day 14 or day 24, what matters most is catching it and understanding it. With consistency, patience, and the right support, your path to pregnancy can stay on track, no matter when ovulation decides to show up.
Frequently Asked Questions About Late Ovulation
Late ovulation typically means ovulating after cycle day 21 in a standard 28-day cycle.
Absolutely. As long as ovulation occurs and intercourse is timed to your fertile window, pregnancy is possible.
Not necessarily. Occasional late ovulation is normal and doesn’t always mean reduced egg quality. Consistently late ovulation may indicate hormonal imbalances worth checking with your doctor.
Yes. Stress, illness, or sudden lifestyle changes can delay ovulation by affecting hormone regulation—but this delay is usually temporary.
References
Su HW, Yi YC, Wei TY, Chang TC, Cheng CM. Detection of ovulation, a review of currently available methods. Bioeng Transl Med. 2017 May 16;2(3):238-246. doi: 10.1002/btm2.10058. PMID: 29313033; PMCID: PMC5689497.
Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. 2003 Sep;18(9):1959-66. doi: 10.1093/humrep/deg366. PMID: 12923157.
Filicori M, Butler JP, Crowley WF Jr. Neuroendocrine regulation of the corpus luteum in the human. Evidence for pulsatile progesterone secretion. J Clin Invest. 1984 Jun;73(6):1638-47. doi: 10.1172/JCI111370. PMID: 6427277; PMCID: PMC437074.



