You’ve been testing with OPKs for days past your usual ovulation window. Still negative. Your period is late, but the pregnancy test is negative too. Sound familiar?
The truth is: yes, stress can delay ovulation, sometimes by just a few days, other times by several weeks. Research published in Human Reproduction shows that stress can disrupt the hormonal signals that trigger ovulation, finding that women with the highest levels of physiological stress biomarkers—such as the enzyme alpha-amylase (sAA)—took 29% longer to conceive compared to those with lower stress levels.
If you’re feeling anxious about this delay (which, ironically, can make things worse), you’re not alone. Understanding why this happens, and what you can do about it, can help you feel more in control of your cycle again.
Can Stress Really Delay Ovulation?
Yes, stress can directly impact the hypothalamic-pituitary-ovarian (HPO) axis, the communication pathway between your brain and reproductive organs.
Think of your HPO axis like a carefully timed relay race: the hypothalamus in your brain, starts by releasing GnRH, which triggers the pituitary, also in your brain, to send out FSH and LH down to your ovaries. Stress is like a false start, it throws off the sequence and delays the baton pass that signals ovulation.
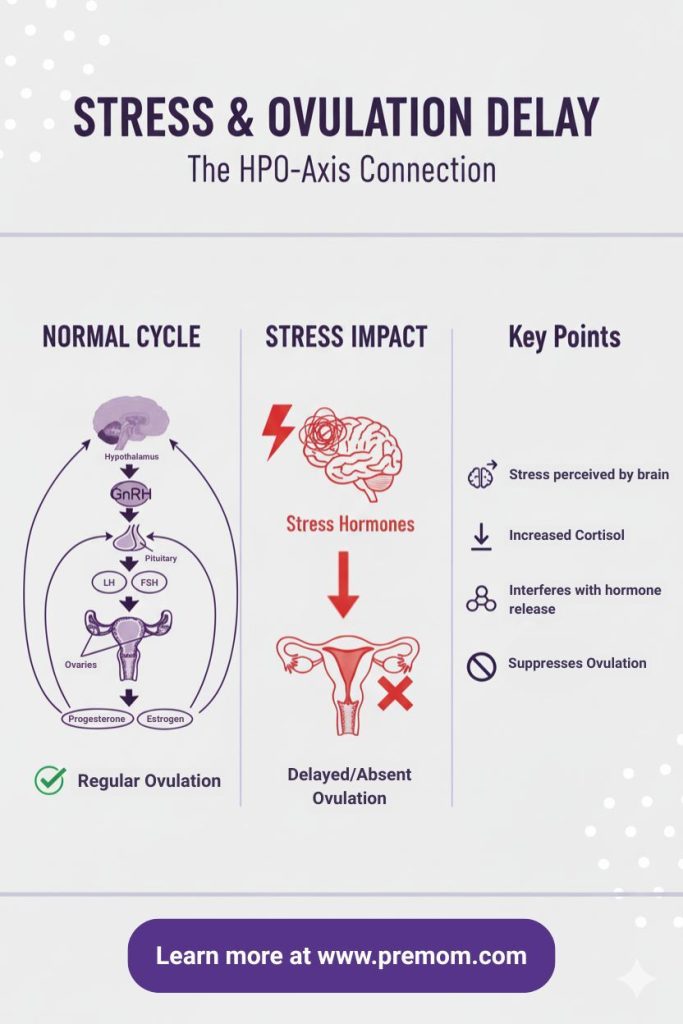
When cortisol levels rise (often above 15–20 µg/dL in sustained stress), the brain suppresses GnRH pulses. Without that rhythm, FSH and LH can’t rise properly, preventing follicle development or the LH surge needed to release an egg.
Types of Stress and Their Impact
- Acute stress (like a big presentation or argument): may delay ovulation by only a day or two.
- Chronic stress (ongoing work pressure, caregiving, or fertility anxiety): may delay ovulation for weeks or even stop it temporarily.
- TTC-related stress: creates a feedback loop, worrying about ovulation may further delay ovulation.
Not All Stress Affects Ovulation the Same Way
If you’ve had stressful months but still ovulated on time, that’s because everyone’s stress resilience is different. Genetics, hormone sensitivity, and lifestyle habits all play a role.
For some women, their cycles are remarkably stable, even under intense stress. For others, even mild emotional or physical strain can throw things off balance. Understanding your unique threshold.and learning to track it, can help you adapt your routine before stress causes major disruption.
Tools like the Premom app can help you identify your personal stress threshold by correlating life events with cycle changes over time.
The Science Behind Stress and Fertility
The Hypothalamic-Pituitary-Ovarian (HPO) Axis Explained
The HPO axis runs on hormonal communication:
- The Hypothalamus releases GnRH (gonadotropin-releasing hormone).
- The Pituitary Gland responds by secreting FSH (follicle-stimulating hormone) and LH (luteinizing hormone).
- The Ovaries use those signals to grow follicles and trigger ovulation.
This delicate chain reaction depends on stable hormone feedback loops, and stress interferes at the very first step.
Where Cortisol Interrupts the Process
When you’re under chronic stress, cortisol suppresses GnRH, reducing FSH and LH output. This can:
- Lower LH surge amplitude
- Delay follicle growth
- May affect egg maturation and quality
The result? Ovulation gets pushed back, or skipped altogether.
Why Your Body Does This (Evolutionary Perspective)
From an evolutionary standpoint, your body interprets chronic stress as a threat, similar to famine or danger. In “survival mode,” reproduction takes a back seat.
While today’s stressors (emails, bills, traffic) aren’t life-threatening, your biology can’t tell the difference. That’s why your body sometimes hits pause on ovulation when life feels overwhelming.
How Long Can Stress Delay Ovulation?
For most women, mild stress might delay ovulation by a few days, but chronic stress can delay it for weeks. It’s the follicular phase (the first half of your cycle) that changes. The luteal phase, the 12–14 days after ovulation, stays relatively consistent.
If you normally ovulate on cycle day (CD) 14 but this month it’s CD 24, your period will also shift about 10 days later.
👉 Related read: No LH Peak: Is It Missed or Late Ovulation?
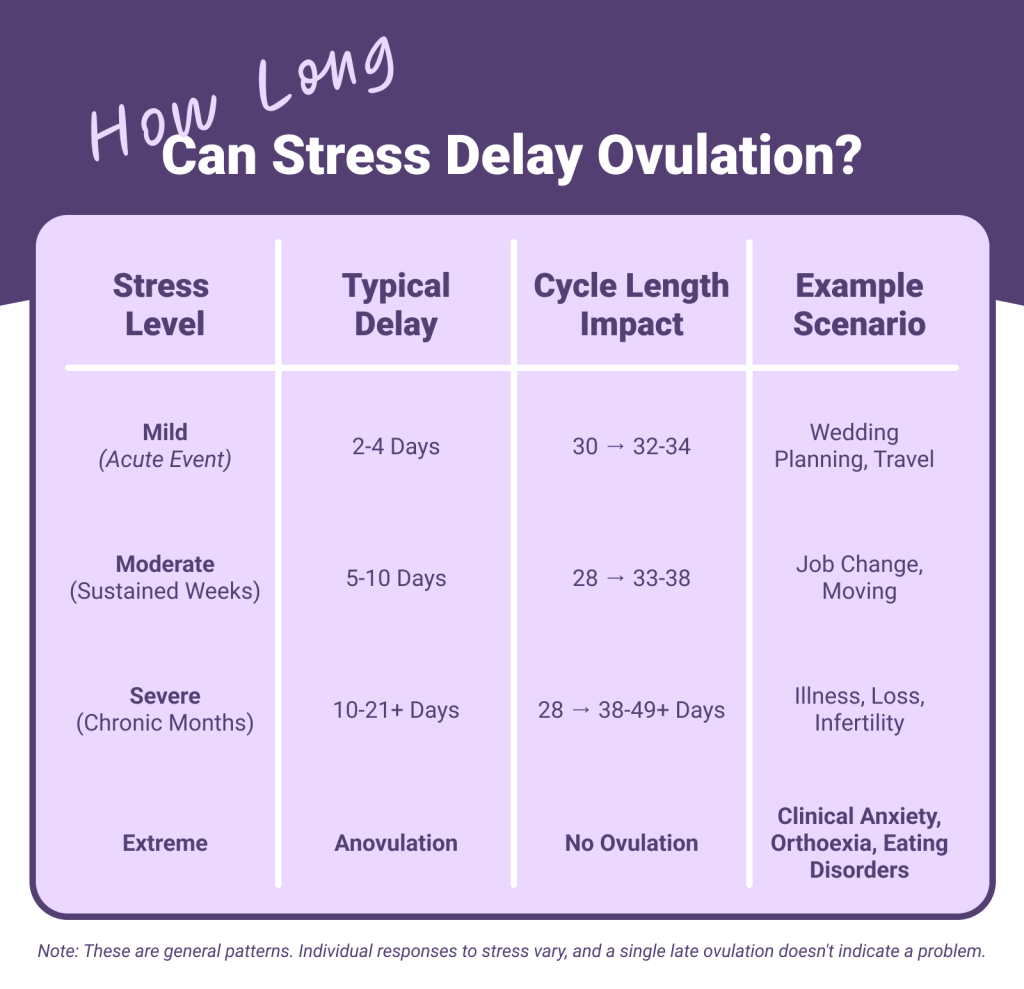
These examples show how varied “normal” can be, so if you recognize your own pattern here, know that you’re not alone.
How to Know If Stress Is Delaying Your Ovulation
Stress-related ovulation delays often show up as:
- Negative OPKs beyond your usual fertile window
- Longer or unpredictable cycles
- Lack of fertile cervical mucus
- No post-ovulation BBT rise
You might also notice symptoms like fatigue, poor sleep, irritability, or appetite changes, these are all cortisol-driven responses that can interfere with hormone balance.
Tracking these symptoms helps you distinguish between a “late ovulation” and an “anovulatory” cycle
The 3-Cycle Pattern Recognition Method
To truly see if stress is impacting your ovulation, track at least three consecutive cycles. Watch for these patterns:
- Ovulation day fluctuates by more than 5 days between cycles
- LH surges or OPK positives get later each month
- BBT rise still happens, but later than usual
Add a quick stress log to your tracker, note major life events, work changes, or emotional shifts. You may start seeing direct links between stress spikes and delayed ovulation.
Stress vs. Other Causes: How to Tell the Difference
Not every irregular cycle is stress-related. Here’s how to tell them apart:
| Cause | Typical Pattern | Other Symptoms |
|---|---|---|
| Stress | Delay varies month-to-month | Sleep, appetite, fatigue |
| PCOS | Consistently irregular or long cycles | Acne, dark hair growth, high LH |
| Thyroid imbalance | Short or long cycles | Weight gain/loss, sensitivity to temp, hair loss, dry skin |
| Perimenopause | Progressive lengthening | Hot flashes, shorter luteal phase, irregular cycles |
If your irregular cycles match the stress column but resolve once life calms down, that’s a good sign your body is responding naturally.
Stress and Late Ovulation — The Catch-22 of TTC
Trying to conceive can feel like an emotional roller coaster. Unfortunately, worrying about whether you’re ovulating can actually make it harder to ovulate.
This creates a TTC stress loop:
- Stress delays ovulation.
- Delayed ovulation increases anxiety.
- Anxiety raises cortisol… delaying ovulation again.
Understanding this feedback loop is the first step to breaking it. When you know what’s happening biologically, it’s easier to focus on gentle stress reduction rather than panic.
Breaking the TTC Stress Loop
The key to interrupting this cycle isn’t to “stop caring” about getting pregnant (impossible advice!). Instead, focus on what you can control:
- Control your tracking method: Use reliable tools like Premom’s quantitative OPKs so you’re not second-guessing faint lines or timing.
- Control your information intake: Limit symptom-spotting and cycle comparison in the two-week wait. Set specific times to check your app rather than obsessively refreshing.
- Control your support system: Join the Premom community where thousands of women share similar experiences. Knowing you’re not alone reduces anxiety’s physiological impact.
Remember: Being stressed about TTC doesn’t make you a failure. It makes you human.
3 Natural Ways to Get Your Cycle Back on Track
1. Lower Cortisol Through Strategic Stress Management
You don’t need to “eliminate stress” (that’s impossible), but you can lower cortisol with targeted methods proven to help women TTC:
- Fertility yoga & breathing: Studies show yoga can reduce cortisol by up to 30% and improve ovulation regularity. Try gentle yoga or the 4-7-8 breathing technique: inhale 4s, hold 7s, exhale 8s.
- Cognitive Behavioral Therapy (CBT): Helps break negative thought loops around TTC.
- Nature time & light exposure: Spending about 20 minutes in natural morning sunlight helps regulate circadian rhythms by supporting a healthy rise in cortisol and enhancing serotonin production, which promotes alertness and a positive mood throughout the day.
- What not to do: Don’t add “relaxing” as another to-do list item. It’s okay to feel stressed, what matters is giving your body safe moments to reset. Consider journaling or talking with your partner to get worries off of your mind.
2. Support Your Cycle with Targeted Nutrition
Your hormones are built from nutrients, so feeding your body well supports recovery.
Cycle Support Foods:
- Magnesium: dark chocolate, pumpkin seeds (400 mg/day)
- Omega-3s: salmon, walnuts, chia (1000 mg EPA/DHA)
- Vitamin B6: chickpeas, bananas (50–100 mg/day)
These help regulate cortisol and support healthy progesterone after ovulation.
Foods to limit: excess caffeine, alcohol, and added sugars, these elevate cortisol and insulin, which can worsen hormonal stress.
3. Track Smarter with Premom’s Adaptive Algorithm
When stress makes ovulation unpredictable, guessing can lead to missed fertile windows. That’s where the Premom app helps. Premom’s adaptive algorithm adjusts to irregular cycles, detecting subtle LH surges and shifting fertile window predictions automatically. By logging LH, PdG, BBT, and cervical mucus together, the app helps you see clear patterns, even when ovulation varies by weeks.
When you can see your LH rising (even if slowly), it reduces the anxiety of wondering ‘did I miss it?’ – and that stress reduction itself can help your body throughout the ovulation cycle.
You can also use Premom’s AI insights to analyze your hormone ratios and visualize your fertile window, helping you time sex more accurately and reduce stress from uncertainty.
Can You Still Get Pregnant with Stress-Delayed Ovulation?
Yes! This is one of the most important things to understand: delayed ovulation doesn’t reduce your pregnancy chances once ovulation occurs.
Ovulation Timing vs. Egg Quality
Many women worry that late ovulation signals poor egg quality. Here’s the truth:
Occasional late ovulation (like CD 21-25 after a stressful month) typically doesn’t affect egg quality at all. Your body simply took longer to mature a follicle, but the egg released is just as viable.
Consistently very long cycles (regularly >35 days) may sometimes correlate with reduced egg quality in research, but this is usually related to underlying conditions like PCOS rather than stress alone.
Your Fertile Window Just Shifts Later
The key principle: Your fertile window moves with ovulation, but the timeline stays the same.
- If you normally ovulate CD14, your fertile window is CD9-14
- If stress delays ovulation to CD24, your fertile window shifts to CD19-24
The 6-day fertile window doesn’t shrink or disappear—it just happens later in your cycle.
Success Rates with Late Ovulation
What matters for pregnancy success isn’t which cycle day you ovulate—it’s whether the key conditions for conception are met:
1. Ovulation occurs (indicated by positive OPK + BBT rise or PdG spike)
2. Luteal phase is adequate (12-14 days to support implantation)
3. Sex is well-timed during the fertile window (5 days before through ovulation day)
Your fertile window shifts with ovulation but doesn’t disappear. If you ovulate on CD14, your fertile window is CD9-14. If you ovulate on CD24, your fertile window is CD19-24. The 6-day window remains the same—it just occurs later.
The bottom line: Late ovulation is a timing challenge, not a fertility problem. When you track accurately with tools like Premom, you can identify your actual fertile window and time sex appropriately—no matter when ovulation happens.
Many women in the Premom community share success stories of conceiving with ovulation on CD25, CD30, or even later. The key was detecting that late ovulation, not eliminating it.
When to Seek Professional Help
If stress-related delays become consistent, it’s time to check in with your healthcare provider.
See a doctor if:
- You haven’t confirmed ovulation for 3+ cycles
- Your cycles are consistently >35 days
- You’ve lost >10% body weight recently or show signs of disordered eating
- You’re over 35 and have been TTC for 6+ months with irregular cycles
- You notice physical symptoms like excess hair growth, acne, or pelvic pain
What to Expect at Your Appointment
Your healthcare provider may:
- Order blood tests to check FSH, LH, progesterone, and cortisol levels
- Perform a transvaginal ultrasound to assess follicle development
- Discuss your stress levels and mental health support options
- Recommend stress reduction techniques or, if needed, fertility medications
Come prepared: Bring your Premom tracking data showing at least 3 cycles. Visual charts showing late or absent ovulation patterns help your doctor make faster decisions.
Premom also offers in-app consultations with fertility nurses and specialists for personalized feedback. Take your Health and Fertility Assessments in the Premom app to understand how stress may be affecting your cycle.
The Bottom Line — Stress and Ovulation
Yes, stress can delay ovulation—and it’s more common than you think. If you’ve experienced a late cycle during a tough month, your body isn’t broken. It’s responding exactly as designed: protecting you when it perceives a threat.
The empowering truth: You don’t need perfect zen to be able to ovulate. You just need to:
- Understand what’s happening in your body
- Track consistently so you know when ovulation occurs
- Lower cortisol when possible through gentle, proven methods
- Time sex based on real data, not calendar guesses
For most women, once acute stressors resolve, cycles return to baseline within 1-2 months. In the meantime, tools like Premom help you work with your body’s stress response rather than fighting against it.
Remember: Late ovulation doesn’t mean no ovulation. It just means your fertile window is later than usual—and with smart tracking, you won’t miss it.
Download the Premom app to track, test, and get expert support on your fertility journey. Whether ovulation arrives on day 14 or day 27, Premom adapts to your unique cycle—giving you confidence and clarity, no matter what stress throws your way.
Frequently Asked Questions About Stress and Ovulation
Yes, chronic or severe stress can absolutely delay ovulation by two weeks or even more, leading to much longer cycles. This happens because the follicular phase (the time leading up to ovulation) lengthens significantly.
On OPKs, a stress-delayed cycle will show negative results for much longer than usual, past your typical ovulation day. You might keep testing daily and only see a gradual increase in your LH ratio much later in your cycle than expected, or even miss a clear surge if the delay is very prolonged.
No, once the LH surge has begun, ovulation is typically imminent (usually within 12-36 hours). Stress usually affects the initiation of the LH surge and the growth of the follicle before the surge. If you’ve already had a confirmed LH peak, stress won’t stop the egg from releasing.
No, late ovulation itself does not typically mean lower egg quality. The egg that eventually ovulates is usually a healthy, viable egg. Egg quality is more related to overall ovarian health and age, not simply the timing of its release within a cycle.
Yes, severe or prolonged chronic stress can indeed cause anovulation (no ovulation at all) rather than just delayed ovulation. When stress is extreme, the body may completely suppress the hormonal signals needed to mature and release an egg.
This is a common and challenging situation. Focus on strategies that create a sense of control and self-care:
1. Smart tracking with Premom: Reduces guesswork and anxiety about your fertile window.
2. Mindfulness and relaxation techniques: Even 5-10 minutes daily can help (e.g., deep breathing, short guided meditations).
3. Set boundaries: Limit conversations about TTC if they become overwhelming.
4. Seek support: Talk to a trusted friend, partner, or a therapist specializing in fertility stress.
5. Focus on overall well-being: Prioritize sleep, healthy eating, and gentle exercise, regardless of your TTC outcome for the month.
References
Schliep KC, Mumford SL, Vladutiu CJ, Ahrens KA, Perkins NJ, Sjaarda LA, Kissell KA, Prasad A, Wactawski-Wende J, Schisterman EF. Perceived stress, reproductive hormones, and ovulatory function: a prospective cohort study. Epidemiology. 2015 Mar;26(2):177-84. doi: 10.1097/EDE.0000000000000238. PMID: 25643098; PMCID: PMC4315337.
Lynch CD, Sundaram R, Maisog JM, Sweeney AM, Buck Louis GM. Preconception stress increases the risk of infertility: results from a couple-based prospective cohort study–the LIFE study. Hum Reprod. 2014 May;29(5):1067-75. doi: 10.1093/humrep/deu032. Epub 2014 Mar 23. PMID: 24664130; PMCID: PMC3984126.
Nepomnaschy, P. A., et al. (2004). Stress and the menstrual cycle: Cortisol levels and reproductive function in women. American Journal of Human Biology, 16(5), 523–532. https://doi.org/10.1002/ajhb.20057
Stanford JB, White GL, Hatasaka H. Timing intercourse to achieve pregnancy: current evidence. Obstet Gynecol. 2002 Dec;100(6):1333-41. doi: 10.1016/s0029-7844(02)02382-7. PMID: 12468181.



